Ovarian Cancer/Primary Peritoneal
This section will take you through the basics of ovarian cancer diagnosis and treatment. It will introduce you to the care provider specialists who may be part of your treatment team and discuss the different types of treatments for ovarian cancer. This page is designed to help aid you and your support system in better understanding ovarian cancer and current treatments in order to play an active role in understanding your care.
View the information in this section in our brochure, Ovarian Cancer: Your Guide available at the links below.
- Ovarian Cancer: Your Guide Download | Order Brochures
- Cáncer de Ovario: Su Guía (Español) Download | Order Brochures
- Ovarian Cancer: Your Guide (Chinese) Download | Order Brochures

Ovarian Cancer Overview
Cancer occurs when cells in an area of the body grow abnormally. Ovarian cancer is the seventh most common cancer among people with gynecologic systems worldwide. It is important to understand that ovarian cancer is not just one disease and every patient’s experience and specific treatments may differ. There are three major categories of ovarian cancer: epithelial ovarian cancer, germ cell cancer, and stromal cell cancer, and there are numerous types of epithelial and stromal cancers.
Types of Ovarian Cancer
Epithelial ovarian cancers are the most common and account for 85% to 89% of ovarian cancers. They form from the surface cells of the ovary or from the fallopian tube surface cells. They rank fourth in cancer deaths among people with gynecologic systems in the U.S. and cause more deaths than any other cancer of the female reproductive system.
Epithelial ovarian cancers can be a part of a hereditary or familial (genetic) syndrome such as those with BRCA1 and/or BRCA2 gene mutations. Fallopian tube and primary peritoneal cancers are also epithelial cancers and have identical behavior, risks and treatment strategies, so are included whenever epithelial ovarian cancer is discussed.
Germ cell cancers are less common forms of ovarian cancer, accounting for only about 5% of ovarian cancers. Germ cell cancers start in the cells that develop into follicles or eggs in the ovaries. This cancer is usually diagnosed in adolescents and young people,and often only affects one ovary.
Equally rare, stromal cell cancers start in the cells that produce female hormones and hold the ovarian tissues together. Similarly, there are several types of stromal cell cancers and presentation and treatment can vary.
Ovarian Cancer Symptoms
Historically, ovarian cancer was called the “silent killer” because symptoms were not thought to develop until the chance of cure was poor. However, recent studies have shown that many symptoms listed below, if new, persistent or worsening, are more likely to occur in people with ovarian cancer than in people with ovaries in the general population. Even patients with early-stage disease may have these symptoms.
These symptoms include:
- Bloating
- Pelvic or abdominal pain
- Difficulty eating or feeling full quickly
- Urinary symptoms (urgency or frequency)
While these may be common symptoms many people without cancer may have occasionally, patients with ovarian cancer report that symptoms are persistent and often progressive, and represent a change from normal for their bodies. The frequency and/or number of such symptoms are key to consider. People who have these symptoms almost daily for more than a few weeks should see their doctor, preferably a gynecologist and have a pelvic (gynecologic) exam. Prompt medical evaluation may lead to earlier detection and more prompt diagnosis and treatment.
Several other symptoms have been commonly reported by people with ovarian cancer. These other symptoms include fatigue, indigestion, back pain, pain with intercourse, constipation or diarrhea, and menstrual irregularities. However, these other symptoms are also found in equal frequency in people with gynecologic systems in the general population who do not have ovarian cancer. Importantly, if a symptom does not go away and gets worse over time, that person should be evaluated by a health care provider.

Medical Evaluation and Diagnosis
When a person experiences concerning symptoms, a pelvic (gynecologic) exam and a general physical exam should be performed. Based on the findings of the exam, imaging of the pelvis with a pelvic ultrasound is often recommended if there is a mass or cyst felt on exam. Even if the exam is normal, people may be recommended to undergo a pelvic ultrasound to evaluate the ovaries.
If an abnormality of the ovaries is found or if the physical exam or symptoms are more concerning, additional imaging tests such as a CT scan or an MRI may be ordered to help your provider understand more about what is happening elsewhere in the body.
Often if there is a mass or complex cyst or something abnormal on the ovaries, blood tests known as tumor markers may be ordered, such as a blood test for a protein called CA 125. Keep in mind that CA 125 is not approved for this use, and is only useful at best for serous cancers.
CA 125 should not be used as a routine screening test, but may help your provider in the work up of a cyst or mass. CA 125 can be elevated in approximately 80% of people with advanced-stage epithelial ovarian cancer, but elevations can occur also for reasons other than ovarian cancer especially in people before menopause.
For more information, please visit foundationforwomenscancer.org for a brochure entitled, CA 125 Levels: Your Guide.
CA 125 is less likely to be elevated in some of the other less common ovarian cancer types (germ cell or stromal cell cancers). Other tumor markers blood tests for these cancer types may be ordered based on a patient’s age, symptoms and imaging findings.
If ovarian cancer is suspected or diagnosed, it is important to seek care first from a gynecologic oncologist—medical doctors with specialized training in treating gynecologic cancers who can manage your care from diagnosis to completion of treatment. Use our Seek a Specialist tool to find a gynecologic oncologist in your area.
During your treatment, you will come in contact with many health care professionals—these people make up your treatment team. They will work with each other and you to provide the special care you need. Learn more about your treatment team.
Ovarian Cancer Staging
When ovarian cancer is diagnosed, it is important to determine if the cancer has spread beyond the ovaries. Your treatment team may do more imaging tests and a biopsy or a. surgery to determine the stage or where the cancer is located. Staging helps to determine the exact extent of your cancer and what treatment plan is best for you.
In some patients, Imaging such as CT scan or MRI scan, can demonstrate spread of the cancer beyond the ovaries or pelvis and the gynecologic and medical oncologists on your treatment team may recommend getting a biopsy, piece of tumor, to confirm that you have ovarian cancer followed by initiation of medical treatment. Surgery is generally put off until after three to four cycles of treatment.
If imaging such as a CT scan shows findings that suggest the cancer may have spread beyond the ovaries, a sample of cancer cells may be obtained through a CT-guided biopsy, ultrasound-guided fluid collection from the abdomen (paracentesis) or space between the lung and chest wall (thoracentesis), or through a laparoscopic surgery. The diagnosis of ovarian cancer must be confirmed by pathologists who look at the biopsies or fluid samples. This information will also help to determine the order of the treatments your team has planned. If the extent of cancer is more advanced or in areas that are difficult to remove medical (chemotherapy) treatment may be started first and a surgery performed later once tumors have shrunk. This approach is called neoadjuvant chemotherapy.
For some patients, a more extensive staging surgery can be performed first instead as part of both the staging and initial cancer treatment plan. This includes a surgery that removes the ovaries, uterus, possibly other organs such as sections of bowel, and ideally all of the visible tumor. This is often called cytoreductive or debulking surgery and is then followed by chemotherapy.
Your team will use all the information from the exam, imaging, biopsy results or any surgery to determine the stage of the cancer. Stages can include: Stage I, II, III, or IV, as illustrated below. The cancer tissue collected will also be assigned a grade. Grade refers to how abnormal the cells appear under a microscope. Low grade tumors, also called grade 1, have features that resemble normal ovarian cells and tend to be slower growing cancers. In contrast, in high grade tumors (grade 3) the microscopic appearance is greatly altered from normal and these cancer cells tend to
grow at a faster rate.
It is important that your staging and/or debulking surgery be performed by a gynecologic oncologist, a physician with special training in the care of ovarian cancers. Studies show that patients treated by gynecologic oncologists at high volume centers have improved outcomes.
Ovarian Cancer Stages
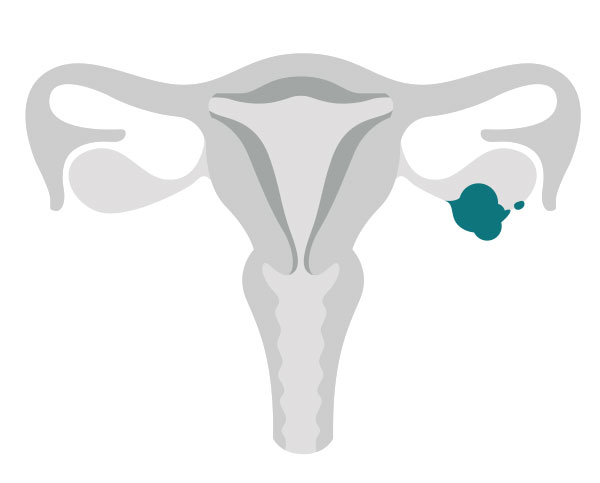
Stage 1:
The cancer is found in one or both ovaries. Cancer cells also may be found on the surface of the ovaries or in fluid collected from the abdomen.
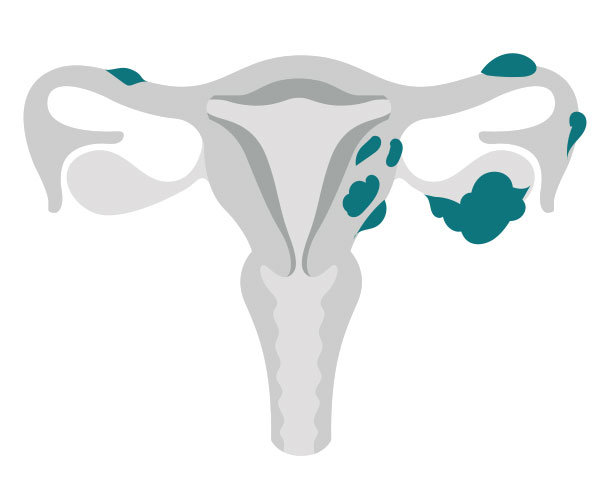
Stage 2:
The cancer has spread from one or both ovaries to other tissues in the pelvis, such as the fallopian tubes or uterus. Cancer cells may also be found in fluid collected from the abdomen.
Stage 3:
The cancer has spread outside the pelvis or nearby lymph nodes. Most commonly the cancer spreads to the omentum (an apron of fatty tissue that hangs down from the colon and stomach), diaphragm, intestine, and the outside (surface) of the liver.
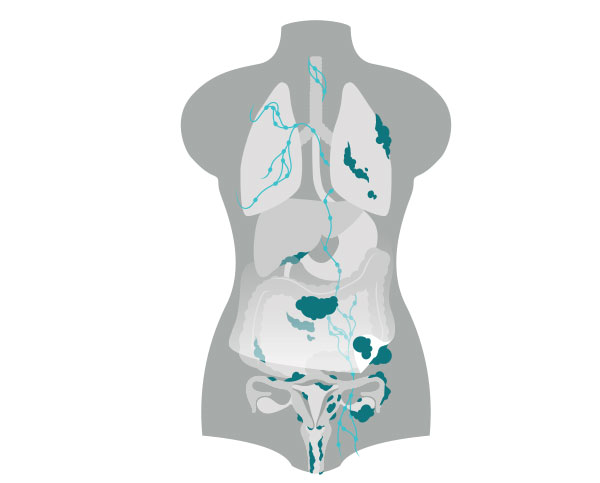
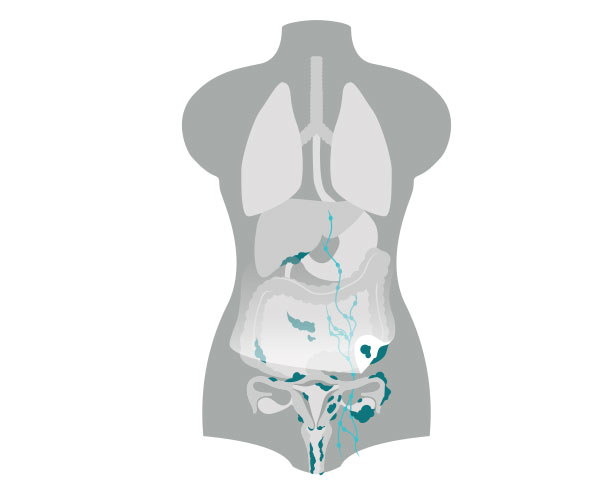
Stage 4:
The cancer has spread to tissues outside the abdomen and pelvis. The most common place for the cancer to spread is in the space around the lungs. Additionally, if the cancer spreads inside the liver or spleen, it is considered stage IV.
Ovarian cancer treatment and side effects
Ovarian cancer is most often treated with surgery and chemotherapy. Whether surgery or chemotherapy is used first will depend on several factors specific to your disease. Only rarely is radiation therapy used. It is important to distinguish between early-stage ovarian cancer and advanced disease because the treatment approaches are different. Different ovarian cancer types may also have different treatments.
All treatments for ovarian cancer have side effects. Most side effects can be managed. Treatments may affect unexpected parts of your life, including your function at work, home, intimate relationships, and deeply personal thoughts and feelings.
Before beginning treatment, it is important to learn about the possible side effects, and talk with your treatment team members about your feelings or concerns. They can prepare you for what to expect and tell you which side effects should be reported to them immediately. They can also help you find ways to manage the side effects that you experience.
Understanding the goals of treatment
As you begin your treatment, make sure that you understand what to expect. Is this for cure? What are the chances of cure? If there is no cure, will the treatment make me live better or longer? It is very important to understand the truth about what to expect from the treatment—and what are the potential costs of side effects, expenses, etc.—so that you can make the best decisions for yourself and the life you want to lead.

Ovarian Cancer Treatment Options
Follow-Up After Treatment
In general, people are followed up with exams (including a pelvic exam) every 3 to 4 months for 3 years, and then every 6 months. In addition, CA 125 and imaging studies such as x-rays, CT scans, or MRIs may be periodically performed, especially if you have any new pains or symptoms.
Recurrent Disease
Recurrences are often diagnosed when the CA 125 level begins to rise, or new masses are found on imaging studies or by examination. A biopsy may be required to be certain a lesion is a recurrent tumor.
If ovarian cancer recurs, there are several options for treatment. These include repeat surgery, re-treatment with the same chemotherapy given initially, treatment with a different type of agent (chemotherapy, hormonal or targeted therapy), and sometimes radiation or a combination of approaches. As each recurrence will be different, it is important to discuss your individual situation with your team. It is also important to investigate whether there is a clinical trial that is appropriate for you. Don’t be afraid to seek a second opinion.
Importance of Participation in Clinical Trials
There are many ongoing clinical trials studying new and better ways to treat ovarian cancer. Many treatment options are available today because women diagnosed with ovarian cancer were willing to participate in prior clinical trials.
Clinical trials are designed to test some of the newest and most promising treatments for ovarian cancer. The Foundation for Women’s Cancer partners with NRG Oncology (formerly Gynecologic Oncology Group), part of the National Cancer Institute cooperative group working only on gynecologic cancer clinical trials, and others to make information about current clinical trials available. For more information about clinical trials available for enrollment, visit ClinicalTrials.gov.
Primary Peritoneal Cancer (PPC)
Cancer occurs when cells in an area of the body grow in an abnormal way. Primary peritoneal cancer (PPC) is a relatively rare cancer that develops most commonly in women. PPC is a close relative of epithelial ovarian cancer, which is the most common type of malignancy that affects the ovaries. The cause of primary peritoneal cancer is unknown, but it is important for women to know that it is possible to have primary peritoneal cancer even if their ovaries have been removed.
The abdominal cavity and the entire surface of all the organs in the abdomen are covered in a cellophane-like, glistening, moist sheet of tissue called the peritoneum. It not only protects the abdominal organs, it also supports and prevents them from sticking to each other and allows them to move smoothly within the abdomen. The cells of the peritoneal lining develop from the same type of cell that lines the surface of the ovary and fallopian tube for that matter. Certain cells in the peritoneum can undergo transformation into cancerous cells, and when this occurs, the result is primary peritoneal cancer. It can occur anywhere in the abdominal cavity and affect the surface of any organ contained within it. It differs from ovarian cancer because the ovaries in PPC are usually only minimally affected with cancer.

Fallopian tube cancer
The fallopian tubes are a pair of floppy tube-like structures that originate at the top (fundus) of the uterus where they communicate with the endometrial cavity and course away from the uterus, on either side, towards the ovaries where they “flop” over the ovaries with their finger-like (fimbriated) end. Cancers of the fallopian tube are also relatively rare and very closely related to cancers of the ovary and PPC. They share many commonalities and emerging data is even suggesting that many of the previously felt to be ovarian cancers may indeed have been Fallopian Tube Cancer (FTC).
Although the clinical presentation of FTC is very similar to ovarian cancer and PPC, there are some differences. Cancers of the fallopian tube arise within the inside (lumen) of the fallopian tube and typically cause it to swell like a sausage. The involvement of the ovary is secondary, but it is usually so extensive that one cannot tell whether it began on the ovary and spread to the fallopian tube, or vice versa. Because of that, many fallopian tube cancers may have been classified as ovarian cancers. As the fallopian tube swells with cancer, it produces fluid, similar to ascites, that can “leak” back into the uterus and lead to a watery vaginal discharge, the classic presentation of FTC when associated with an adnexal mass.
PPC and FTC symptoms
Unfortunately, because of the vague nature of the signs, PPC and FTC are usually diagnosed in advanced stages of disease, when achieving a cure is difficult.
The typical symptoms of both are more commonly gastrointestinal rather than gynecologic in nature, and include:
- Abdominal bloating
- Changes in bowel habits
- Early feeling of fullness after eating
- Bloating and when severe, nausea and vomiting may result
Occasionally, patients can present with a blockage of the intestines related to tumor on or next to the bowels. Vaginal bleeding is infrequently seen in patients with PPC, but may be a little more common in patients with FTC.
Medical Evaluation and Diagnosis
Both PTC and FTC are usually diagnosed when a woman sees her doctor complaining of abdominal swelling and bloating. As described above, the symptoms of either cancer are more commonly gastrointestinal than gynecologic in nature. These symptoms are related to the accumulation of fluid, also known as ascites, that commonly occurs with either cancer. Gastrointestinal symptoms also occur because seedlings of tumor often line the peritoneal surface (the outer lining) of the intestines, a process called carcinomatosis. The omentum, an apron of fatty tissue that hangs down from the colon and stomach, often contains bulky tumor, described as omental caking. Although omental cakes can be detected on a physical exam, they frequently are subtle and difficult to detect. When a woman is found to have fluid in the abdomen (ascites), the usual first step toward a diagnosis is a CT scan. This is a special type of x-ray test that allows doctors to assess the entire abdomen and pelvis. Omental caking and ascites, as well as other tumor growths, are commonly seen, and point toward the diagnosis of PPC, FTC or ovarian cancer. Other cancers can cause these findings, thus, further tests are needed and are usually focused around ruling out other more common cancers, such as colon and breast cancer.
Frequently, the evaluation of ascites begins with a procedure known as a paracentesis, whereby fluid is removed from the abdomen using a needle. The fluid is examined under the microscope, looking for the presence of cancerous cells. Unfortunately, this procedure is not without risks as the process of performing a paracentesis can actually “seed” the abdominal wall with cancer cells. Therefore, it is important to seek the advice of a gynecologic oncologist when considering this procedure as it may not be necessary given that most patients with these findings will undergo surgery regardless of the results. However, it may be helpful in the patient who is either not a surgical candidate, or in one suspected of having ascites for reasons other than cancer, such as liver or heart disease. Sometimes fluid is even drawn off because of patient discomfort until surgery or chemotherapy can be scheduled.
There are several blood tests that are frequently performed when either PPC or FTC is suspected. The most common of which is the CA 125 blood test. CA 125 is a chemical that is made by tumor cells and is usually elevated in patients with PPC and FTC. Unfortunately, it can also be elevated in a variety of benign conditions, as well as other cancers, and thus an elevated CA 125 blood test does not mean the patient has a cancer. More recently a newer blood test, HE4, can also be used as it is less likely elevated than CA 125 in benign conditions. You can read more about CA 125 with our brochure, CA 125 Levels: Your Guide.
The actual diagnosis of PPC or FTC is often not completely certain until a woman undergoes surgery. This is because the clinical presentation of either disease is so similar to that of epithelial ovarian cancer. PPC, FTC and ovarian cancer appear identical under the microscope. It is the pattern of tumor distribution and organ involvement in the abdominal cavity that indicates the origin of the primary cancer. Patients with FTC usually have gross involvement of the fallopian tubes with lesser involvement of the ovaries. Patients with PPC are usually found to have normal ovaries, or only superficial involvement of the ovaries, at the time of pre-surgical imaging tests or at time of surgery. However, the diagnosis can occasionally remain uncertain even following surgery.
Surgical Staging
Surgical staging of cancers is performed in order to fully assess the extent of disease. This allows for decisions to be made regarding additional therapy, which is usually in the form of chemotherapy. Surgical staging generally involves removal of all visible disease, as well as removal of the ovaries, fallopian tubes and uterus. It can also include removal of the omentum, lymph nodes and other organs depending on the surgical findings.
While there is no formal agreed-upon staging system for PPC, because it is so similar to ovarian cancer with respect to treatment, tumor state is typically assigned using guidelines established for ovarian cancer.
Stages I through IV describe how far the tumor has spread. Nearly all patients diagnosed will have Stage III or higher because warning signs are typically few until the cancer is widespread. Patients with PPC or FTC may have fluid around the lungs, known as a pleural effusion. If an effusion is present, some fluid may be removed in order to look for tumor cells. If tumor cells are found in this fluid, the patient has Stage IV disease.
PPC and FTC treatment side effects
Both PPC and FTC are treated in the same way as ovarian cancer is treated. They are most often treated with surgery and chemotherapy—only rarely is radiation therapy used. Your specific treatment plan will depend on several factors, including:
- Stage and grade of the cancer
- Size and location of the cancer
- Your age and general health
All treatments for either cancer have side effects. Most side effects can be managed or avoided. Treatments may affect unexpected parts of your life, including your function at work, home, intimate relationships and deeply personal thoughts and feelings.
Before beginning treatment, it is important to learn about the possible side effects and talk with your treatment team members about your feelings or concerns. They can prepare you for what to expect and tell you which side effects should be reported to them immediately. They can also help you find ways to manage the side effects you experience.

PPC and FTC treatment options
Follow up after treatment
After initial treatment is completed, patients with either cancer are followed closely with visits every two to four months for the first three years and then every six months for another two years or so and ultimately yearly. At each visit they have a physical exam, including a pelvic exam, CA 125 testing, and, depending on the patient and her situation, imaging tests, such as CT scans, X-rays, MRIs or PET scans, may be performed. Unless patients are diagnosed early these cancers have a tendency to recur with time. Hence, patients often require more than one round of chemotherapy and may also need additional surgical procedures.
Recurrent disease
Recurrences are common in patients with PPC or FTC because most patients with either cancer are diagnosed when they already have advanced stages of disease. The majority of patients will initially go into remission, but the disease commonly returns months to years later when the CA 125 levels begins to rise, or new masses are found on physical exam or imaging studies. Unfortunately, the prognosis for this cancer is not favorable once it recurs, but a longer remission before recurrence is associated with a better chance for a second, third and even fourth remission.
There are several treatment options for patients who recur, depending on the location of recurrence, time since the initial therapy and the patient’s overall health status. These options include repeat surgery, re-treatment with the same chemotherapy that was given initially or a different type of agent. Radiation therapy can also be considered for selected cases. Each recurrence is different, so their treatment must be individualized based on a variety of factors including those listed above. Unfortunately, once a recurrence is diagnosed, one must re-focus the goals of treatment to help prolong quality of life rather than a cure.