Vaginal Cancer
This section will take you through the basics of what you need to know about vaginal cancer. It will introduce you to the people who may be part of your treatment team and identify the different types of treatments for vaginal cancer. Hopefully, this information will help prepare you to talk with your treatment team and to feel more confident about your treatment plan.
View the information in this section in our brochure, Vulvar and Vaginal Cancers: Your Guide available at the links below.
- Vulvar and Vaginal Cancers: Your Guide Download | Order Brochures
- Cáncer de Vulva y de Vagina: Su Guía (Español) Download | Order Brochures
- Vulvar and Vaginal Cancers: Your Guide (Chinese) Download | Order Brochures

Vaginal Cancer Overview
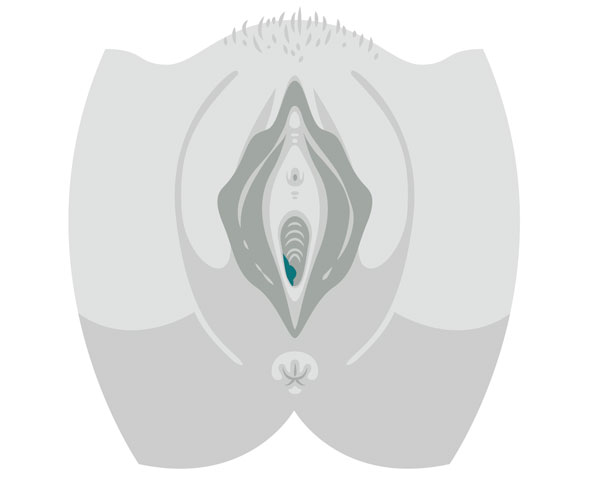
Vaginal cancer begins in the vagina, the muscular tube, also called the birth canal, that connects the outer genitalia to the uterus. Most of these cancers are in the lining (squamous epthelilum) of the vagina and usually affect people between 50-70 years old. Primary vaginal cancer is one of the rarest gynecologic cancers as oftentimes cancer cells found in the vagina originate from the uterus, vulva, or other organs.
Because many vaginal cancers are associated with the Human Papillomavirus (HPV) types 16 and 18, vaginal cancer can be prevented by the vaccinations advocated for the prevention of cervical cancer.
Types of Vaginal Cancers
There are four types of vaginal cancer, depending on where the cancer began.
Vaginal squamous cell carcinoma is the most common type and refers to the thin, flat cells that line the surface of the vagina.
Vaginal adenocarcinoma begins in the glandular cells on the surface of the vagina.
Vaginal melanoma develops on the pigment-producing cells of the vagina.
Vaginal sarcoma develops in the connective tissue cells or smooth muscle cells in the vagina walls.
Vaginal Cancer Symptoms
Vaginal cancer, especially at the precancerous and early stages, may not cause any symptoms.
Common signs for more advanced vaginal cancer include:
- Unusual vaginal bleeding (i.e., between menses, after intercourse, new postmenopausal
bleeding) - Pain (vaginal, vulvar, lower abdominal/pelvic, back or flank)
- Problems with urination or bowel movements
- Watery vaginal discharge
- Lump or mass in the vagina

Medical Evaluation and Diagnosis
Vaginal cancer can be found during a routine pelvic examination. To detect this cancer, people sometimes are given a Pap test to look for abnormal cells, an inspection of the vagina with a special lighted microscope and/or sample (biopsy) of the vaginal tissue for testing.
If vaginal cancer is suspected or diagnosed, it is important to seek care first from a gynecologic oncologist—medical doctors with specialized training in treating gynecologic cancers who can manage your care from diagnosis to completion of treatment. Use our Seek a Specialist tool to find a gynecologic oncologist in your area.
During your treatment, you will come in contact with many health care professionals—these people make up your treatment team. They will work with each other and you to provide the special care you need. Learn more about your treatment team.
Surgical Staging
In general, cancers are divided into categories or stages, with the assignment with a stage based on the risk for recurrence.
Vaginal Cancer Stages
Stage 1:
The cancer is found only in the vaginal wall.

Stage 2:
The tumor has spread to the tissue next to the vagina.

Stage 3:
The cancer has spread to the lymph nodes or the pelvis.

Stage IVA:
In addition to spreading to nearby lymph nodes, the cancer also has spread to the bladder, rectum or pelvis

Stage IVB:
The cancer has spread beyond the vagina to areas like the lungs.
Vaginal cancer treatment and side effects
Most patients with vaginal cancer are treated with surgery or radiation therapy.
Vaginal Cancer Treatment Options
Importance of Participation in Clinical Trials
There are many ongoing clinical trials studying new and better ways to treat gynecologic cancers. Many treatment options are available today because people diagnosed with gynecologic cancers were willing to participate in prior clinical trials.
Clinical trials are designed to test some of the newest and most promising treatments for gynecologic cancers. The Foundation for Women’s Cancer partners with NRG Oncology (formerly Gynecologic Oncology Group), part of the National Cancer Institute cooperative group working only on gynecologic cancer clinical trials, and others to make information about current clinical trials available. For more information about clinical trials available for enrollment, visit ClinicalTrials.gov.